Responding to a Concern
Amendment
In March 2024, a new Section 10. If the Adult has Died was added. It contains information previously located in the Disclosure and Raising a Concern Procedure.
This procedure should be used by safeguarding practitioners and managers when a concern has been raised and a decision needs to be made about whether or not to move to an enquiry, or to take any other action that may be more appropriate and proportionate.
Check the Contacts and Practice Resources area for any supplementary guidance or processes you are required to follow when responding to a concern/referral.
All of the overarching aims, duties and principles of adult safeguarding apply when a concern is raised and decisions need to be made about how best to respond. These are:
- The aims of adult safeguarding;
- The duty to promote individual Wellbeing;
- The six key principles of all adult safeguarding;
- Making Safeguarding Personal; and
- The principles of the Mental Capacity Act.
Abuse and neglect can occur in many ways and the same type of abuse can have a different effect on one adult when compared to another. Hence it is not appropriate to have set responses based on the type of abuse that has occurred and the response should be based on the effect on the adult.
Depending on the information available any number of responses could be deemed appropriate. This could be a single response or a combination of responses. For example:
- The provision of information and advice (relating to the risk of abuse and how the adult may protect themselves, the presenting issues of the situation e.g. financial advice or any other care and support matter);
- A referral to police where a criminal act appears to have taken place (for example theft or assault);
- A referral to a service, for example an NHS service (for example community nursing) or a specialist support organisation (for example Women's Aid);
- A referral to another adult care and support service (for example a prevention service or a service that is able to carry out a needs assessment or a carers assessment);
- A non-statutory enquiry or statutory enquiry under Section 42 of the Care Act (where further information gathering is required to make a decision about an appropriate response or where the nature of the concern requires a formal or multi-agency approach).
The Lead Safeguarding Practitioner receiving the concern is responsible for gathering all of the information necessary to answer the questions and address the matters set out in subsequent sections of this procedure:
- Section 5: Urgent Questions;
- Section 6: Does the Safeguarding Duty Apply?
- Section 7: Other Matters for Consideration;
- Section 8: Making a Decision; and
- Section 9: Establishing the Need for Independent Advocacy
Note: Where an online form has been completed much of this information should already have been provided.
|
Details of the person raising the concern |
|
|
Details of the adult |
|
|
Information about the abuse or neglect |
|
|
Details of the person alleged to have caused harm |
|
|
Immediate actions taken to protect the adult from harm |
|
The concern, and all information gathered should be recorded in line with local recording requirements.
If the adult (or others) is in immediate danger steps should be taken to remove the source of harm, or to remove them from the source of harm.
For example, where an adult is at risk of harm in a care home they may be able to visit family, or it may be necessary to move them (or the adult causing the harm) to another service.
The emergency services should be contacted immediately if the adult (or others) is in immediate danger and cannot be removed from the source of harm. The person handling the concern should contact the emergency services on 999.
When an adult appears to be in need of urgent medical attention they should be advised (and assisted if appropriate) to go to the nearest A & E department.
If necessary, A & E staff should consult with, and involve, relevant clinical specialists about diagnosis, treatment and investigation to establish the cause of symptoms.
If the adult is not in immediate danger then consideration should still be made as to priority of response.
If this is the case the Police should be notified as a priority, if they have not already been contacted by the person raising the concern.
This can be done without the adult's consent if there is a reasonable belief that notifying the police would be in the public interest.
The duty to safeguard an adult applies when all of the following criteria is met:
- The adult has needs for care and support (whether these have been assessed or are being met by the local authority or not);
- They are experiencing, or at risk of experiencing abuse or neglect; and
- As a result of care and support needs they are unable to protect themselves against the abuse or neglect.
If all of the above criteria is met the duty to safeguard applies and a formal safeguarding enquiry under S42 of the Care Act is likely to be the most appropriate response.
1. The adult has needs for care and support
The safeguarding duty applies regardless of whether a person's care and support needs have been formally assessed or not. It also does not matter who is providing or commissioning any care and support services.
For example:
- Services commissioned by adult services;
- Services commissioned by children's services (e.g. a 0-25 team or education services);
- Services commissioned by the NHS (e.g. in a hospital or through NHS Continuing Healthcare);
- Informal support from a carer; and
- Services arranged and funded by the adult or their family.
An adult with care and support needs may be:
- An older person;
- Someone with mental health needs, including dementia or a personality disorder;
- A person with a long-term health condition;
- Someone who misuses substances or alcohol to the extent that it affects their ability to manage day-today living.
Consideration of this need for care and support must be person-centred (for example, not all older people will be in need of care and support but those who are 'frail due to ill health, physical disability or cognitive impairment' may be). The above is not an exhaustive list and it must be considered alongside the impact of needs on the adult's individual wellbeing.
There are 10 areas of potential need (outcomes) set out in the Care Act;
- Manage and maintain nutrition;
- Maintain personal hygiene;
- Manage toilet needs;
- Being appropriately clothed;
- Be able to make use of their home safely;
- Maintain a habitable home environment;
- Develop/maintain family and other personal relationships;
- Access/engage in work, training, education or volunteering;
- Make use of community services;
- Carry out caring responsibilities for a child.
Based on the information provided, if there is any chance at all that the adult may have needs for care and support in any of these areas, this condition should be deemed as met.
2. The adult is experiencing, or at risk of experiencing abuse or neglect
Practitioners should not limit their view of what constitutes abuse or neglect, as it can take many forms.
Responses and decisions should be based on the specific circumstances and take into consideration the actual or potential impact on the adult's individual wellbeing together with their view about the impact that the abuse or neglect has had upon them.
The Care Act 2014 sets out 10 specific categories of abuse and neglect.
The diagram below sets out factors that might be considered in making the necessary judgements about 'reasonable cause to suspect'; and whether the situation reflects the statutory criteria:
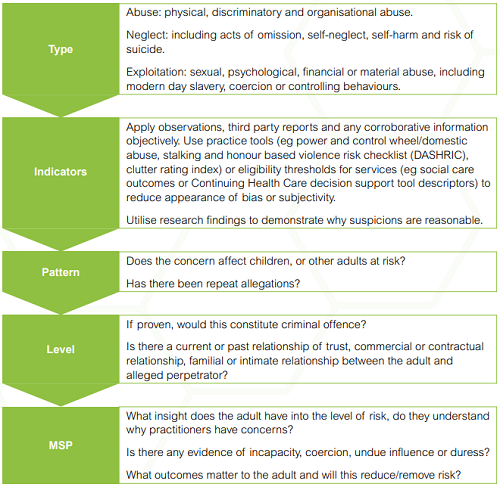
Diagram source: Making decisions on the duty to carry out Safeguarding Adults enquiries (Local Government Association).
For information about these categories, and examples of how the accompanying abuse or neglect may be experienced, see: The Care Act 2014, Categories of Abuse and Neglect.
3. As a result of care and support needs, the adult is unable to protect themselves against the abuse or neglect
Potential barriers to an adult's ability to protect themselves might include:
- They do not have the skills, means or opportunity to self-protect;
- They may have a disability which impairs their capacity to make decisions about protecting themselves or may need support to enact decisions;
- They live in a group setting where they lack control over the way they are treated or the environment;
- There is a power imbalance;
- They may not understand an intention to harm them;
- They may be trapped in a domestic situation which they are unable to leave, or where coercion and control means they cannot make a decision about doing so;
- Their resilience and resourcefulness to protect themselves from harm is eroded by, for example, coercive control and / or a high risk environment.
If any of the safeguarding criteria is not met, the adult is not an 'adult at risk' as defined in the Care Act and the duty to undertake safeguarding enquiries under S42 does not apply.
However, the Care Act permits action to be taken to provide support to the adult by carrying out a non-statutory enquiry where it believes doing so is the most appropriate and proportionate response to the circumstances.
The appropriate Manager should decide what, if any, other action is appropriate and proportionate to the presenting circumstances. Where further action is required the appropriate Manager must ensure that this is taken. For example, a referral to a specialist support service or intervention by a social work team.
Where a decision is made to carry out a non-statutory enquiry this should be undertaken in the same way as a statutory enquiry.
Anyone raising a concern should always seek consent of the adult before doing so, unless:
- Seeking consent will increase the level of risk posed to them (or a child or other vulnerable adult); or
- When consent cannot practically be sought (for example, the referrer is being denied access to the adult or the adult cannot be located in a timely way);
- The adult lacks capacity to consent, and a decision has been made that raising a concern is in their best interests.
If it is not clear from the concern raised whether or not consent has been sought the practitioner handling the concern should contact the person that raised the concern to establish this.
If they are not contactable (for example if the concern was raised anonymously) the practitioner handling the concern should work on the basis that consent was not sought.
The reasons that the person raising the concern did not seek consent should be clearly recorded in line with local recording requirements.
If none of the above conditions apply then the adult must be contacted, advised that a concern has been raised and asked about their wishes in regards to next steps. This can be done by the person that raised the concern or the Lead Agency, whichever is deemed most appropriate and proportionate to the presenting circumstances.
It is only appropriate to make enquiries without consent if:
- 'Vital interests' are at stake;
- The adult is being subjected to inhuman or degrading treatment which is having a serious impact on their wellbeing;
- Other adults or children are at risk of being abused;
- There are concerns that decision has not been made freely but been unduly influenced or subject to coercive control.
Note: 'Vital interests' generally apply to life or death situations and serious, immediate concerns for safety.
In cases where the adult has capacity to withhold consent the Lead Agency should ensure that any intervention is limited to that which is necessary to reduce the risk of harm.
In line with the overarching aims, duties and principles of adult safeguarding, the Lead Agency must have regard for the views and wishes of the adult when deciding the outcome. In particular, whether the adult has expressed any outcomes that, as a consequence of the safeguarding referral they:
- Want to achieve;
- Want to change; or
- Want to stay the same.
The views and wishes of the adult should be clearly recorded in line with local recording requirements.
Note: If the adult has expressed a clear view or wish about what the outcome should be the decision made by the Lead Safeguarding Practitioner should reflect this wherever possible.
It is important as part of the decision making process that the impact on the adult in question is understood. This will ensure that the response is appropriate and proportionate to their specific circumstances.
Impact includes;
- Nature of the risk of harm (physical, emotional or otherwise);
- Likelihood (and frequency) of the harm occurring;
- Severity of harm should it occur;
- Effectiveness of any current risk reduction measures; and
- Impact on individual Wellbeing domains.
Note: When assessing the likelihood of harm occurring this should be an evidence based judgement.
If circumstances are having a significant impact on the adult the local authority intervention required is likely to be more urgent and intensive.
The locally developed Safeguarding and Quality Guidance should be used to support decisions about impact and risk. It can be found in the Contacts and Practice Resources area.
An adult's vulnerability is determined by a range of interconnected factors, including personal characteristics, factors associated with their situation or environment and social factors.
Some of these factors are described below:
| Personal Characteristics of the adult that may increase vulnerability may include: | Personal Characteristics of the adult that may decrease vulnerability may include: |
|---|---|
|
|
| Social/situational factors that increase the risk of abuse may include: | Social/situational factors that decrease the risk of abuse may include: |
|
|
It is important to ascertain whether or not there have been previous safeguarding concerns raised in respect of the adult in question.
Although the existence of previous concerns must not dictate the decision of the current concern, they can provide a great deal of intelligence and information. In particular, they can help determine whether the person is experiencing sustained abuse and which approaches to support them may be most/least effective.
Some key questions:
- Is the nature of the abuse or neglect the same?
- Is the person alleged to be causing harm the same?
- What was the previous response to the concerns?
- What was effective/ineffective about the previous response/s?
- What do previous concerns indicate about the person's ability to engage with the safeguarding process?
Note: In no circumstances should repeat concerns be seen as sole justification for case closure.
For further guidance see: Repeated Allegations Procedure
Where gaps in information remain and the duty to instigate an enquiry is not clear, the subsequent decision should be to move to enquiry.
Any information shared should be:
- Necessary for the purpose for which it is being shared;
- Shared only with those who have a need for it;
- Accurate and up to date;
- Shared in a timely fashion;
- Shared accurately;
- Shared securely.
The Care Act 2014 is clear that all safeguarding decisions and actions must be made in a timely and proportionate way, based on the presenting circumstances.
In order to ensure all responses are timely the SAB requires referral decisions to be made as quickly as possible, taking into consideration the views, wishes and feelings of the adult where possible.
The appropriate Manager/Advanced Practitioner is responsible for making the decision about moving the concern onto the enquiry stage.
Practitioners involved in steps 4, 5, 6 and 7 above are responsible for making a professional recommendation to the appropriate Manager / Advanced Practitioner and ensuring that they have access to all relevant information upon which to base their decision.
Note: If the appropriate Manager/Advanced Practitioner is not available, they should designate an appropriate colleague to deputise in their absence.
The decision should be clearly recorded in line with local recording requirements.
The record should be clear about the rationale behind decision made and how the views and wishes of the adult have been regarded.
Adult previously aware
In all cases, if the adult knew a concern was being raised, they must also be informed of the decision that has been made.
This can be done by the person that raised the concern or the Lead Agency, whichever is deemed most appropriate and proportionate to the presenting circumstances.
The person informing the adult should also:
- Speak to them about likely next steps;
- Ascertain how they wish to be an active part of the safeguarding process;
- Establish whether they will have 'substantial difficulty' engaging with any aspect of the safeguarding process, and whether the duty to provide independent advocacy applies.
If the adult does not wish to be present (in person or virtually) in any subsequent meetings or discussions, their views and wishes in relation to desired outcomes should be sought.
For further information about independent advocacy, see Section 9, Independent Advocacy.
Adult not aware-Decisions to make enquiries
If the adult was not aware of the safeguarding concern (because one or more of the conditions set out in section 6. above was met), they must now be told of the concern and the decision made to move to enquiry.
This is important because, without doing so, the overarching aims and principles of safeguarding adults cannot be applied.
The method of alerting the adult should be carefully considered, to take into account potential risk factors and distress. For example;
- When to speak with them (best time of day, location);
- Who should speak with them (person that raised the concern, practitioner, health professional, existing advocate);
- How to speak with them to ensure maximum understanding (in person, face to face, use of easy read material);
- Any support they may need during or after the conversation;
- Any additional strategies that may need to be implemented to reduce risk afterwards.
Only in exceptional circumstances, where speaking with the adult would increase the risk of abuse can the appropriate Manager decide not to alert them at this stage of the process and instead, move to appoint an independent advocate on the basis that they would find it substantially difficult to engage.
For further information about independent advocacy, see Section 9, Independent Advocacy.
Adult not aware-Decisions to close the case
If the adult was not aware of the safeguarding (because one or more of the conditions set out in Section 6. above was met) then it is not necessary to inform them that the case has been closed unless there is need to discuss any other action with them. For example, the provision of information and advice or whether they would consent to a referral to another social care or health team.
Where concerns were raised by an organisation or professional, the person that raised the concern should be notified of the decision made, even if they are not likely to be involved in any subsequent enquiry or Safeguarding Plan. This will allow them to keep accurate records.
Where concerns were raised by a member of the public, they should be given adequate information to satisfy them that their concerns have been acted upon, but that does not breach confidentiality or compromise any ongoing process or enquiries.
All information sharing should be carried out with regard to the Caldicott Principles, Data Protection legislation and local information sharing policies.
If an enquiry (S42 or non-statutory) is to be instigated an initial discussion will be the first course of action. This will determine what initial actions are required, by whom and how quickly.
See: Safeguarding Discussions and Meetings Procedure, Discussions.
If a decision is made that an enquiry is not appropriate the concern should be closed.
Any external supporting documents (for example Disclosure Reports) must be stored in line with Data Protection legislation and local recording policy. They should also be stored in a logical manner so they can be easily accessed should the information be requested by legal services or the police.
If anybody (the adult or any other person or professional) is dissatisfied with the decision made they can discuss their concerns with the appropriate Manager or make a formal complaint.
Professionals and agencies should refer to the Multi-Agency Escalation Policy and Procedure.
Whenever the outcome of a safeguarding concern is to instigate a S42 enquiry the local authority has a duty under Section 68 of the Care Act to make an independent advocate available to the adult when:
- There is no appropriate other person to support and represent them; and
- They feel that the adult would experience substantial difficulty being fully involved in the safeguarding process without support.
The Lead Agency also has a power (but not a duty) to make advocacy available in other situations on a case by case basis if it deems this appropriate and is able to do so. For example, when instigating an informal enquiry outside of the S42 duty.
Having substantial difficulty is not the same as lacking mental capacity.
See: The Care Act 2014, Determining Substantial Difficulty for information about how to determine substantial difficulty.
See the Mental Capacity Act 2005 Resource and Practice Toolkit, with guidance about assessing capacity and making best interest decisions.
An appropriate person for general representation purposes is not the same as an appropriate person for independent advocacy under the Care Act.
See: The Care Act 2014, An Appropriate Other Person for information about the difference and how to establish whether there is already an appropriate person.
It is not appropriate for any of the following people to act as an appropriate person:
- They are engaged in providing care or treatment for the adult (in either a professional or paid capacity);
- They are implicated in the safeguarding adults referral;
- The lacks capacity to consent to being represented and supported by them and the local authority does not believe it to be in their best interests;
- The person wishing to represent the adult has demonstrated that they do not have adequate direct contact with them in order to do so effectively;
- The person wishing to represent the adult has demonstrated adequate knowledge of the safeguarding adults process they will be supporting them to be involved in;
- The person wishing to represent the adult has demonstrated they are able to act independently from the Lead Agency;
- The person wishing to represent the adult is not employed by or involved with the Lead Agency in any way;
- There is no conflict of interest or dispute between the adult and the person wishing to represent them; and
- Where the adult lacks capacity there is no conflict of interest or dispute between the person wishing to represent them and the Lead Agency about what is best for the adult.
Note: It is not sufficient for a person wanting to support and represent an adult under the s68 of the Care Act to know them well or love them deeply. They must demonstrate that they are able to support the person to be actively involved with safeguarding adults' process.
The role of an independent advocate appointed under the Care Act is not the same as the role of a general advocate or any other type of advocate (for example an Independent Mental Capacity Advocate or an Independent Mental Health Advocate).
An independent advocate appointed under the Care Act must both facilitate and maximise the involvement of the adult with substantial difficulty in the safeguarding process that is taking place.
For information about the ways in which an independent advocate should fulfil their role, see: The Care Act 2014, The Role of an Independent Advocate.
Adults who lack capacity will likely be legally entitled to advocacy under both the Care Act and the Mental Capacity Act 2005.
The Care Act statutory guidance recognises that it would not normally be appropriate or practical for an adult to have 2 advocates and gives the local authority the responsibility to make a decision about the best type of advocacy support.
There are various factors that should influence this decision (such as existing rapport with an advocate or whether any important decisions are likely to be the outcome of the safeguarding process) and the Lead Agency must ensure that whatever it decides, it does not deny the adult any of the specialist advocacy skills they need or are entitled to.
Adults eligible for an Independent Mental Health Advocate (IMHA) under the Mental Health Act 1983 will likely be entitled to advocacy under the Care Act.
The Care Act statutory guidance recognises that it would not normally be appropriate or practical for an adult to have 2 advocates and gives the local authority the responsibility to make a decision about the best type of advocacy support.
There are various factors that should influence this decision (such as existing rapport with an advocate or the likely outcome of the safeguarding process) and the Lead Agency must ensure that whatever it decides, it does not deny the adult any of the specialist advocacy skills they need or are entitled to.
The advocacy referral can be made at any time and should be made without delay as soon as the duty applies.
The advocacy service in Salford is provided by Mind in Salford.
For information about the service and to make a referral see: Mind in Salford website.
Regardless of whether or not independent advocacy is available in the local area the duty to provide it still applies. A failure to do so is a breach of this duty and of the law. It is the role of commissioners to ensure that advocacy services are in place and available when required, and it is the role of practitioners to make timely referrals to advocates to prevent unnecessary delays in the meeting of its duty.
If you are aware that advocacy support is required and is not yet available, urgent interim measures during planning discussions/meetings may need to be agreed without an advocate in place in order to reduce immediate risk to the adult from inaction. However, you must not proceed to close the safeguarding concern, or make long term or irreversible decisions until it is in place.
The duty upon the Lead Agency is to make independent advocacy support available to any adult who requires it. Once made available the duty is met.
If an adult decides that they do not wish to engage in the advocacy support that has been made available to them they do not have to do so, but the Lead Agency must still provide it.
The Lead Agency is expected under the Care Act to support the adult to understand the role of an advocate and promote its benefit to them so as to reduce the likelihood that they will not engage.
While the section 42 duty does not apply to an adult once they have died, there may be outstanding concerns in relation to risk to others and/or quality concerns related to a collective setting or service. There is a continued responsibility to ensure these are appropriately addressed in accordance with the Care Act and other relevant provisions.
Consideration should be given to each of the following:
- Notification to the police;
- Raising a concern (s) for others at risk;
- Referral for a Section 44 Safeguarding Adults Review;
- Notification to the Care Quality Commission (CQC);
- Notification to the appropriate Commissioning Team; and
- Notification to the Coroner.
Guidance about each of these considerations is provided below.
The police should be notified as a matter of priority if:
- The death of the adult is suspected to have been potentially attributed to abuse or neglect; and/or
- There is reason to suspect that a crime is likely to be committed i.e., other people are at risk.
If the circumstances of the death mean that there are reasons to be concerned about risks to other adults, enquiries may need to be made to decide whether action needs to be taken to protect them. For example, this will often be necessary following a death in an organisational setting where other adults are continuing to receive a service.
If the criteria for a Section 44 Safeguarding Adults Review is met, a Safeguarding Adults Referral must be made.
See: Safeguarding Adult Reviews (SAR) Policy and Procedure.
It is important to remember that a Section 44 Safeguarding Adults Review relates to how safeguarding partners have worked together to safeguard the adult and is not appropriate for single agency issues/failure.
If there are concerns about how a provider has cared for the adult prior to their death a notification should be made to CQC via the CQC website.
The CQC has powers to bring a criminal prosecution against health and social care providers for failing to provide care and treatment in a safe way.
If there are concerns about the quality of care delivered by the provider, the relevant Commissioning Team (Local Authority and/or Integrated Care Board) should be notified. The Commissioning Team can instigate the provider concern process and, if necessary, decommission the provider if appropriate improvements are not made.
Following a death, it is usually a doctor, or the police, who will decide whether a referral to the Coroner is required. When a death has been referred to the Coroner, the Coroner will make decisions regarding whether a police investigation should take place and whether a post-mortem is required.
Further guidance is available on what constitutes a safeguarding adult concern from the LGA/ADASS: Making decisions on the duty to carry out Safeguarding Adults enquiries.
Last Updated: March 6, 2024
v81